Significance
Cardiac arrest remains one of the leading causes of mortality in the United States, with over 500,000 incidents reported annually and a median survival rate of just 18%. In-hospital cardiac arrests (IHCAs) pose distinct challenges for healthcare professionals tasked with responding to these unpredictable events. Despite dedicated efforts, less than 25% of patients experiencing in-hospital cardiac arrest achieve survival.
Models for Intra-Resuscitation Care
The Advanced Cardiac Life Support (ACLS) algorithm, developed by the American Heart Association, serves as the gold standard in managing cardiac arrest. Strict adherence to these protocols is essential for enhancing patient survival rates; however, deviations from established guidelines are unfortunately common. For healthcare providers, understanding and addressing these challenges is crucial in improving survival rates and ensuring the highest standards of care during critical interventions.
Error Accumulation & Effects on Mortality
Research indicates that 41.3% of cardiopulmonary resuscitations involve some form of deviation from ACLS protocols, and the presence of multiple errors during resuscitation can reduce the likelihood of achieving return of spontaneous circulation (ROSC) by nearly 50%. Each additional error compounds on prior errors and further diminishes the chances of ROSC by approximately 30%. Given the already low survival rates, these errors significantly impact patient outcomes.
Sources of Error
The current processes for managing cardiac arrests are often suboptimal, presenting numerous barriers to effective resuscitation efforts. While developing Code Clock, we surveyed 35 hospital clinicians—including physicians, nurses, and EMTs—our findings indicate that clinicians identify errors during cardiopulmonary resuscitation approximately 50% of the time. Additionally, 35% of respondents reported that factors such as chaos, noise, and stress significantly hinder their ability to deliver effective resuscitation.
Typically, around 15 employees from diverse clinical specialties rotate through coverage as part of the “code team.” This diverse composition often leads to team members working in different areas of the hospital, resulting in limited prior interaction and collaboration.
Awareness of these limitations is essential for enhancing the effectiveness of resuscitation efforts and ultimately improving patient outcomes.
Enter: Code Clock
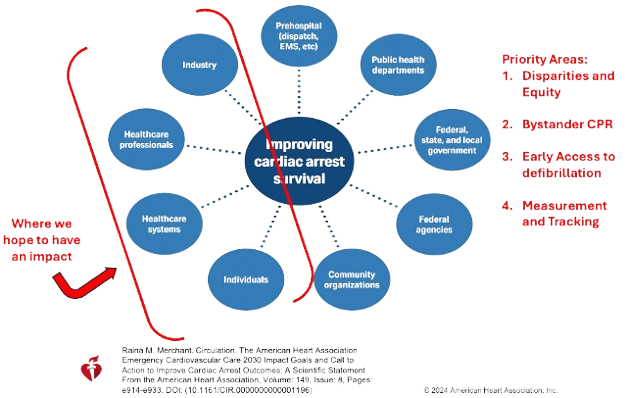
CodeClock was initially developed by clinicians to address key challenges identified by hospital code team members. As part of our comprehensive strategy, we aim to create a series of devices designed to enhance outcomes not only for Advanced Cardiac Life Support (ACLS) but also for Basic Life Support (BLS) and bystander CPR. Our commitment is to improve the effectiveness of resuscitation efforts across all levels of care.