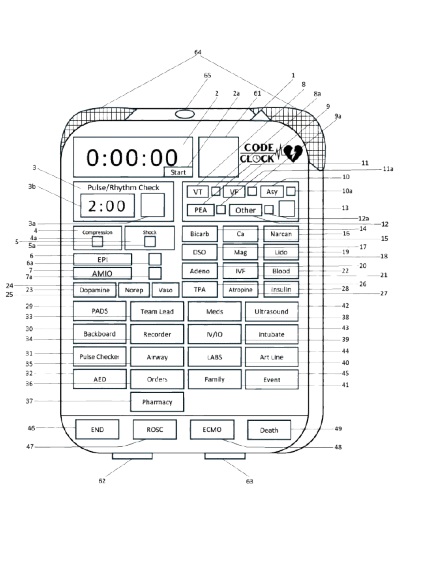
Initial Prototype
Convenient Integration: Code Clock attaches to crash cart for easy access during emergent situations.
Visual Cues: Equipped with flashing lights, the device signals recommended interventions during resuscitation. This feature helps guide the team through critical steps and reduces the risk of missing important actions.
Integrated Timers: The device features both a code duration clock, allowing users to track the overall length of the resuscitation effort, as well as a pulse check timer, which displays the time remaining until the next pulse check.
Organizational Support: Allows the assignment and tracking of roles and tasks within the resuscitation team. This feature helps streamline team coordination and clarifies responsibilities during high-pressure situations.
Accurate Record-Keeping: Facilitates the marking of the time when interventions are administered and denotes the final outcome of the resuscitation effort. This feature aids in maintaining detailed records for quality improvement and post-event analysis.
Developed for and featured at Bench to Bedside through the University of Utah in April 2024, Code Clock’s initial prototype was the recipient of the Patient Safety Award, sponsored by the Pittsburgh Regional Health Initiative and the Jewish Healthcare Foundation.
Features
Size: 12”x15”x4”
Processor: Raspberry Pi Model 4B
Operating System: Raspbian OS
Software: Custom Python script utilizing Adafruit CircuitPython libraries
Specifications
Version 2
Since our initial prototype and competition in April 2024, we've made significant improvements to the Code Clock, enhancing its functionality for healthcare environments. Key upgrades to our working prototype (as of September 2024) include:
Badge Swipe Feature: Healthcare staff can now swipe their badges to log their presence during resuscitation, improving tracking for debriefing purposes.
Battery Life: The device now features a battery with a 2-3 hour charge, ensuring reliability during critical moments.
Compact Design: We've reduced the device size from 12”x15”x4” to 9”x11”x2”, making it more portable and convenient.
Enhanced Functionality: Additional buttons have been added to increase functionality and data collection.
Display Screen: A new screen displays critical information, such as the number of medication rounds administered, allowing clinicians to quickly access vital data.
Device Updates
Future Developments
Our vision for Code Clock encompasses a comprehensive suite of devices tailored to enhance Advanced Cardiac Life Support (ACLS), Basic Life Support (BLS), and bystander assistance during cardiac arrest situations. This initiative will feature three distinct devices, each designed to provide effective support in hospitals, clinics, and emergency field environments.
ACLS
The current working prototype of Code Clock is designed to support Advanced Cardiac Life Support (ACLS) guided care in accordance with the evidence-based protocols established by the American Heart Association. This device is intended for use in hospitals, particularly within critical care settings where trained clinicians are present.
BLS
With a preliminary patent secured and plans to develop a prototype in 2025, the BLS version of Code Clock is designed to enhance the effectiveness of Basic Life Support (BLS) delivered by trained personnel in accordance with American Heart Association standards. This iteration of the device will be particularly beneficial in non-critical care hospital settings, clinics, pre-hospital environments, and various outpatient facilities.
Bystander
With a preliminary patent in place and the intention to prototype in 2025, the bystander version of Code Clock represents a significant advancement in efforts to improve cardiac arrest outcomes. This streamlined version of the device is specifically designed for individuals without formal training in Basic Life Support (BLS) or Advanced Cardiovascular Life Support (ACLS).
By simplifying the process of delivering lifesaving interventions, expanded versions of Code Clock aims to foster confidence and increase the likelihood of effective intervention during cardiac emergencies. Ultimately, the goal is to bridge the gap between emergency response and the immediate care that can be provided by laypersons, thereby enhancing survival rates and outcomes for victims of cardiac arrest.